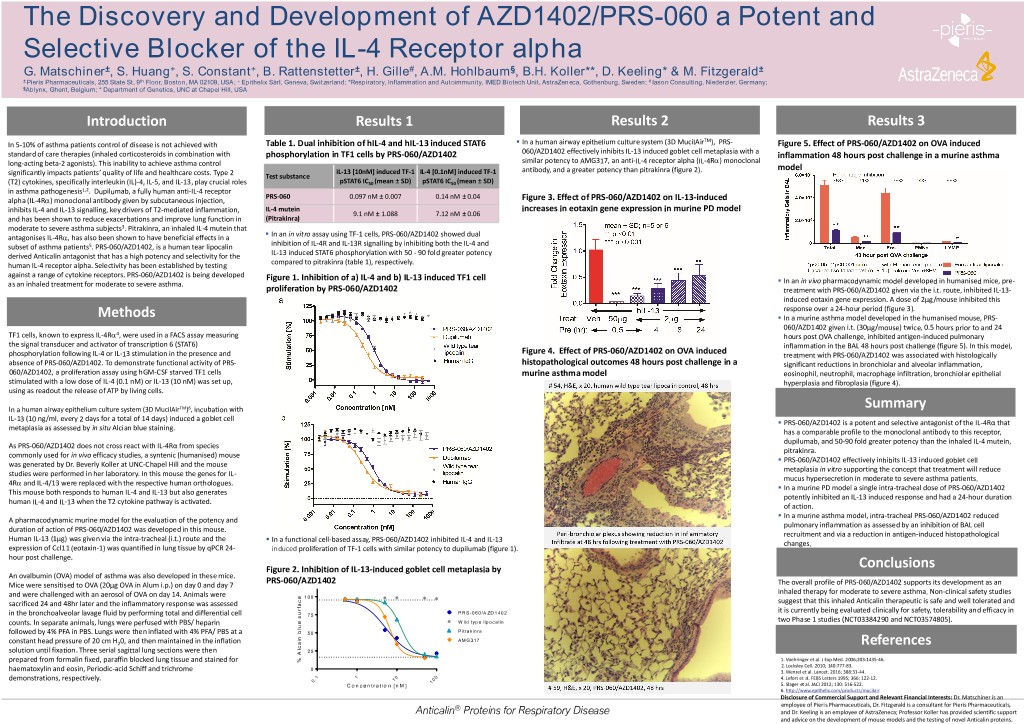
The Discovery and Development of AZD1402/PRS-060 a Potent and Selective Blocker of the IL-4 Receptor alpha G. Matschiner±, S. Huang+, S. Constant+, B. Rattenstetter±, H. Gille#, A.M. Hohlbaum§, B.H. Koller**, D. Keeling* & M. Fitzgerald± ± Pieris Pharmaceuticals, 255 State St, 9th Floor, Boston, MA 02109, USA; + Epithelix Sàrl, Geneva, Switzerland; *Respiratory, Inflammation and Autoimmunity, IMED Biotech Unit, AstraZeneca, Gothenburg, Sweden; # Iason Consulting, Niederzier, Germany; §Ablynx, Ghent, Belgium; * Department of Genetics, UNC at Chapel Hill, USA Introduction Results 1 Results 2 Results 3 ▪ TM In 5-10% of asthma patients control of disease is not achieved with Table 1. Dual inhibition of hIL-4 and hIL-13 induced STAT6 In a human airway epithelium culture system (3D MucilAir ), PRS- Figure 5. Effect of PRS-060/AZD1402 on OVA induced standard of care therapies (inhaled corticosteroids in combination with phosphorylation in TF1 cells by PRS-060/AZD1402 060/AZD1402 effectively inhibits IL-13 induced goblet cell metaplasia with a inflammation 48 hours post challenge in a murine asthma long-acting beta-2 agonists). This inability to achieve asthma control similar potency to AMG317, an anti-IL-4 receptor alpha (IL-4Ra) monoclonal IL-13 [10nM] induced TF-1 IL-4 [0.1nM] induced TF-1 antibody, and a greater potency than pitrakinra (figure 2). model significantly impacts patients’ quality of life and healthcare costs. Type 2 Test substance (T2) cytokines, specifically interleukin (IL)-4, IL-5, and IL-13, play crucial roles pSTAT6 IC50 (mean ± SD) pSTAT6 IC50 (mean ± SD) in asthma pathogenesis1,2. Dupilumab, a fully human anti-IL-4 receptor PRS-060 0.097 nM ± 0.007 0.14 nM ± 0.04 alpha (IL-4Ra) monoclonal antibody given by subcutaneous injection, Figure 3. Effect of PRS-060/AZD1402 on IL-13-induced inhibits IL-4 and IL-13 signalling, key drivers of T2-mediated inflammation, IL-4 mutein increases in eotaxin gene expression in murine PD model 9.1 nM ± 1.088 7.12 nM ± 0.06 and has been shown to reduce exacerbations and improve lung function in (Pitrakinra) moderate to severe asthma subjects3. Pitrakinra, an inhaled IL-4 mutein that ▪ antagonises IL-4Ra, has also been shown to have beneficial effects in a In an in vitro assay using TF-1 cells, PRS-060/AZD1402 showed dual subset of asthma patients5. PRS-060/AZD1402, is a human tear lipocalin inhibition of IL-4R and IL-13R signalling by inhibiting both the IL-4 and derived Anticalin antagonist that has a high potency and selectivity for the IL-13 induced STAT6 phosphorylation with 50 - 90 fold greater potency human IL-4 receptor alpha. Selectivity has been established by testing compared to pitrakinra (table 1), respectively. against a range of cytokine receptors. PRS-060/AZD1402 is being developed Figure 1. Inhibition of a) IL-4 and b) IL-13 induced TF1 cell ▪ as an inhaled treatment for moderate to severe asthma. In an in vivo pharmacodynamic model developed in humanised mice, pre- proliferation by PRS-060/AZD1402 treatment with PRS-060/AZD1402 given via the i.t. route, inhibited IL-13- induced eotaxin gene expression. A dose of 2µg/mouse inhibited this response over a 24-hour period (figure 3). Methods ▪ In a murine asthma model developed in the humanised mouse, PRS- 060/AZD1402 given i.t. (30µg/mouse) twice, 0.5 hours prior to and 24 TF1 cells, known to express IL-4Ra4, were used in a FACS assay measuring hours post OVA challenge, inhibited antigen-induced pulmonary the signal transducer and activator of transcription 6 (STAT6) inflammation in the BAL 48 hours post challenge (figure 5). In this model, phosphorylation following IL-4 or IL-13 stimulation in the presence and Figure 4. Effect of PRS-060/AZD1402 on OVA induced treatment with PRS-060/AZD1402 was associated with histologically absence of PRS-060/AZD1402. To demonstrate functional activity of PRS- histopathological outcomes 48 hours post challenge in a significant reductions in bronchiolar and alveolar inflammation, 060/AZD1402, a proliferation assay using hGM-CSF starved TF1 cells murine asthma model eosinophil, neutrophil, macrophage infiltration, bronchiolar epithelial stimulated with a low dose of IL-4 (0.1 nM) or IL-13 (10 nM) was set up, hyperplasia and fibroplasia (figure 4). using as readout the release of ATP by living cells. In a human airway epithelium culture system (3D MucilAirTM)6, incubation with Summary IL-13 (10 ng/ml, every 2 days for a total of 14 days) induced a goblet cell ▪ PRS-060/AZD1402 is a potent and selective antagonist of the IL-4Rα that metaplasia as assessed by in situ Alcian blue staining. has a comparable profile to the monoclonal antibody to this receptor, dupilumab, and 50-90 fold greater potency than the inhaled IL-4 mutein, As PRS-060/AZD1402 does not cross react with IL-4Rα from species pitrakinra. commonly used for in vivo efficacy studies, a syntenic (humanised) mouse ▪ PRS-060/AZD1402 effectively inhibits IL-13 induced goblet cell was generated by Dr. Beverly Koller at UNC-Chapel Hill and the mouse metaplasia in vitro supporting the concept that treatment will reduce studies were performed in her laboratory. In this mouse the genes for IL- mucus hypersecretion in moderate to severe asthma patients. 4Ra and IL-4/13 were replaced with the respective human orthologues. ▪ In a murine PD model a single intra-tracheal dose of PRS-060/AZD1402 This mouse both responds to human IL-4 and IL-13 but also generates potently inhibited an IL-13 induced response and had a 24-hour duration human IL-4 and IL-13 when the T2 cytokine pathway is activated. of action. ▪ In a murine asthma model, intra-tracheal PRS-060/AZD1402 reduced A pharmacodynamic murine model for the evaluation of the potency and pulmonary inflammation as assessed by an inhibition of BAL cell duration of action of PRS-060/AZD1402 was developed in this mouse. recruitment and via a reduction in antigen-induced histopathological Human IL-13 (1µg) was given via the intra-tracheal (i.t.) route and the ▪ In a functional cell-based assay, PRS-060/AZD1402 inhibited IL-4 and IL-13 changes. expression of Ccl11 (eotaxin-1) was quantified in lung tissue by qPCR 24- induced proliferation of TF-1 cells with similar potency to dupilumab (figure 1). hour post challenge. Figure 2. Inhibition of IL-13-induced goblet cell metaplasia by Conclusions An ovalbumin (OVA) model of asthma was also developed in these mice. Mice were sensitised to OVA (20µg OVA in Alum i.p.) on day 0 and day 7 PRS-060/AZD1402 The overall profile of PRS-060/AZD1402 supports its development as an and were challenged with an aerosol of OVA on day 14. Animals were inhaled therapy for moderate to severe asthma. Non-clinical safety studies e 1 0 0 c suggest that this inhaled Anticalin therapeutic is safe and well tolerated and sacrificed 24 and 48hr later and the inflammatory response was assessed a f r it is currently being evaluated clinically for safety, tolerability and efficacy in in the bronchoalveolar lavage fluid by performing total and differential cell u 7 5 P R S -0 6 0 /A Z D 1 4 0 2 s two Phase 1 studies (NCT03384290 and NCT03574805). counts. In separate animals, lungs were perfused with PBS/ heparin e W ild ty p e lip o c a lin u l b P itra k in ra followed by 4% PFA in PBS. Lungs were then inflated with 4% PFA/ PBS at a 5 0 n i A M G 317 constant head pressure of 20 cm H20, and then maintained in the inflation a References c solution until fixation. Three serial sagittal lung sections were then l 2 5 A 1. Voehringer et al. J Exp Med. 2006;203:1435-46. prepared from formalin fixed, paraffin blocked lung tissue and stained for % 2. Locksley Cell. 2010; 140:777-83. 0 haematoxylin and eosin, Periodic-acid Schiff and trichrome 3. Wenzel et al. Lancet. 2016; 388:31-44. 1 1 0 0 demonstrations, respectively. . 1 0 4. Lefort et al. FEBS Letters 1995; 366: 122-12. 0 1 C o n c e n tr a tio n [n M ] 5. Slager et al. JACI 2012; 130: 516-522. 6. http://www.epithelix.com/products/mucilair Disclosure of Commercial Support and Relevant Financial Interests: Dr. Matschiner is an ® employee of Pieris Pharmaceuticals, Dr. Fitzgerald is a consultant for Pieris Pharmaceuticals, Anticalin Proteins for Respiratory Disease and Dr. Keeling is an employee of AstraZeneca; Professor Koller has provided scientific support and advice on the development of mouse models and the testing of novel Anticalin proteins.